But that’s not the extent of inaccurate claims. We took a deeper look at some of the claims Dr. Wine made when we interviewed him.
Statement: “You will have to have [Lyme disease] for a minimum of nine months before you're ever going to test positive.”
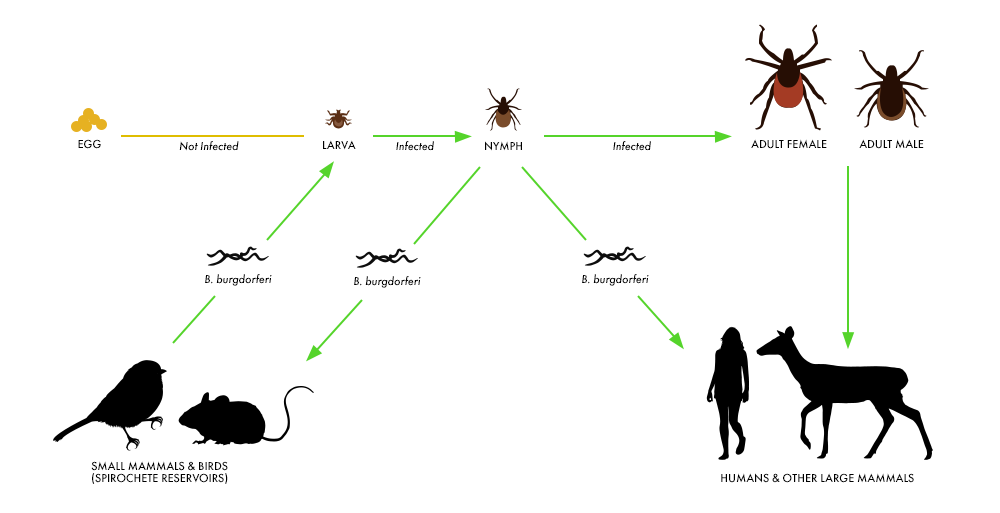
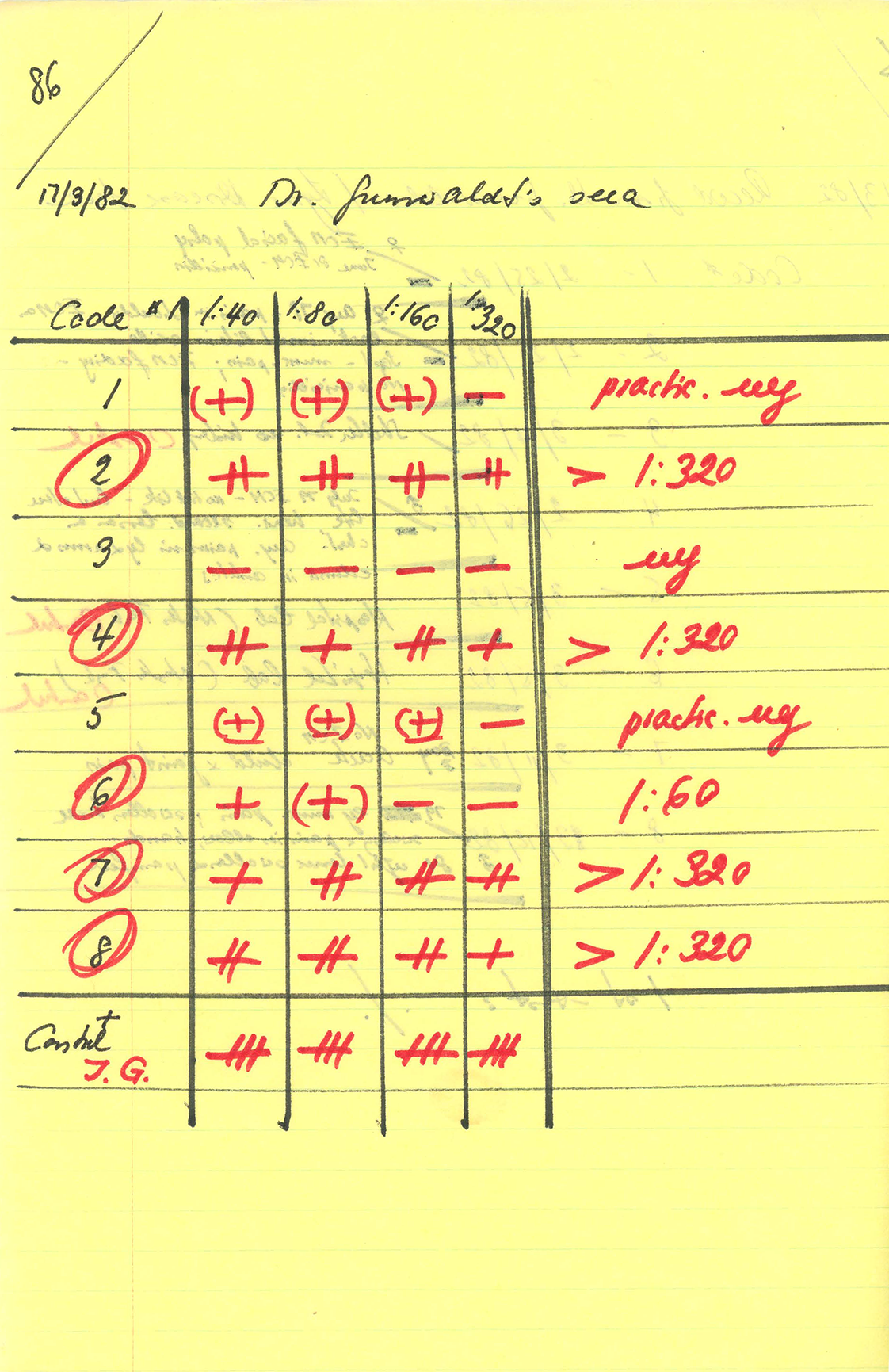
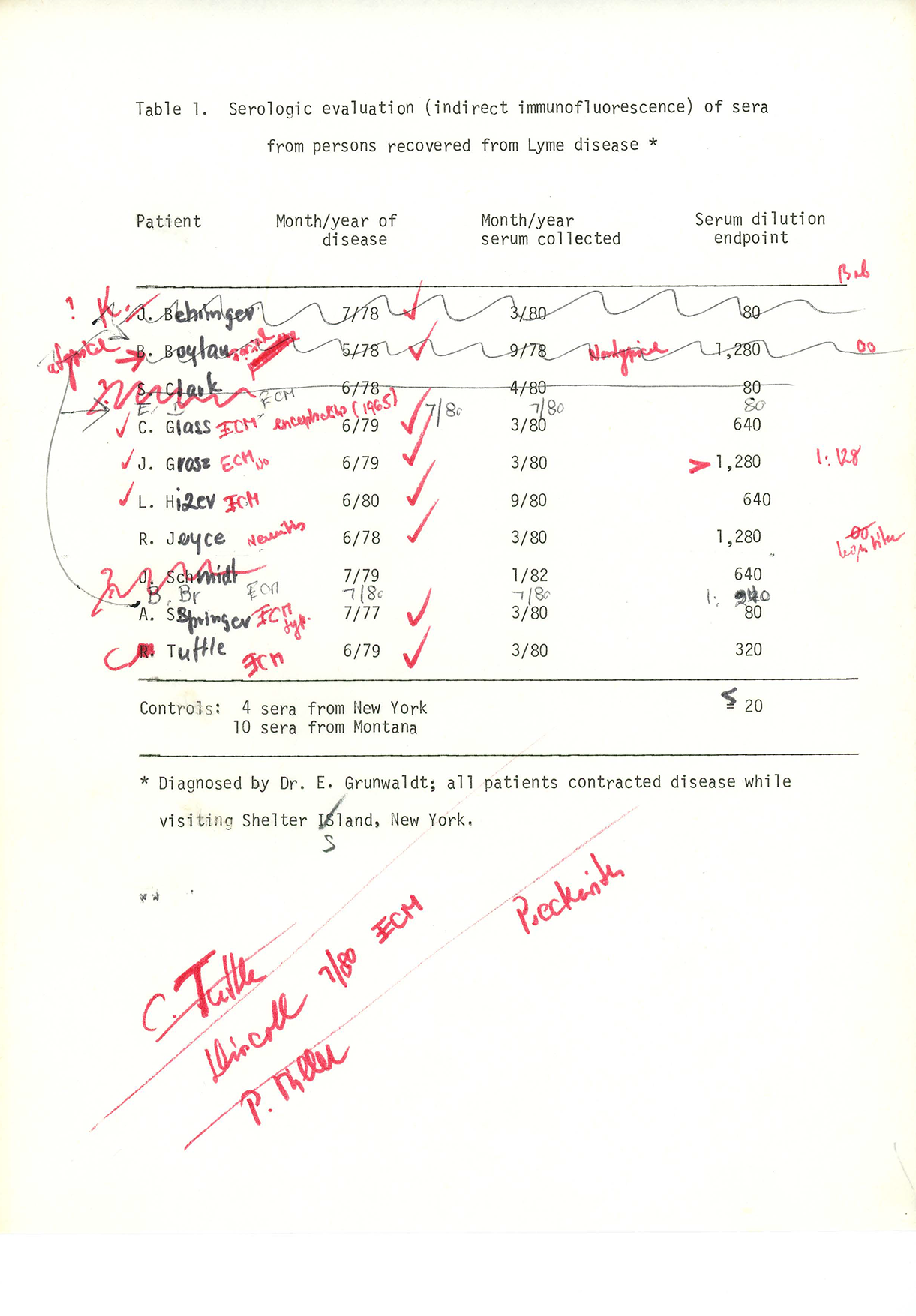
It is true that when you are first bitten by a tick, you will test negative on the standard CDC recommended Lyme disease test. One study found that in the first week after a bullseye appears, less than 1 in 5 patients will have enough Lyme antibodies to register. However in the same study, by three weeks after the appearance of a bullseye, that number rises to 85 percent.
This is why the standard practice is to treat anyone presenting a bullseye rash immediately for Lyme disease. Testing is typically most useful for patients who have “disseminated” Lyme disease — usually months after a tick bite, after the bullseye rash and flu-like illness has disappeared and other symptoms begin to manifest. In patients who have cardiac symptoms, acute neurological symptoms, or the classic “Lyme arthritis” the tests have been found to be 85 to 99 percent accurate.
Statement: “70 percent of all ticks carry the Lyme spirochete.”
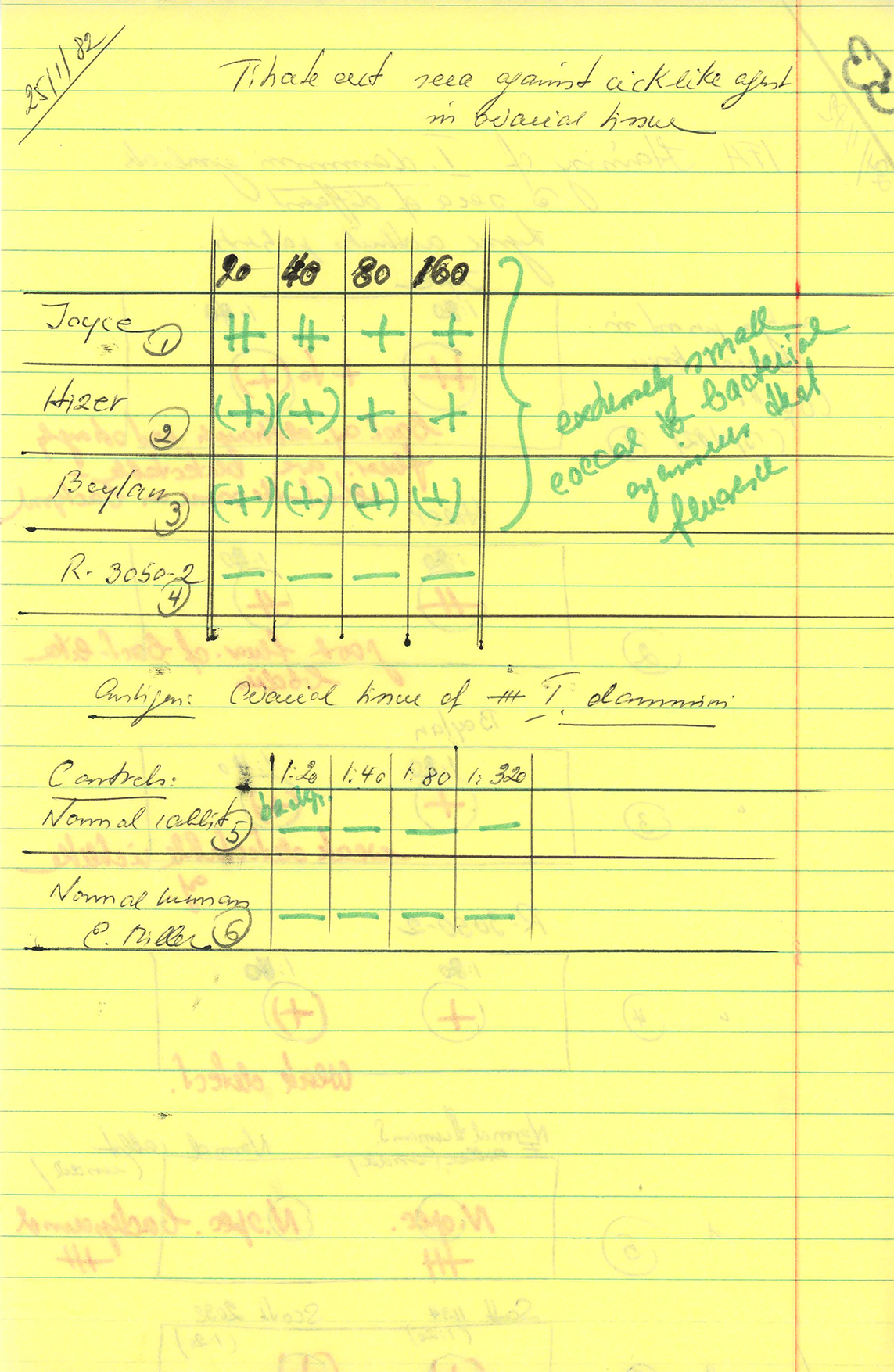
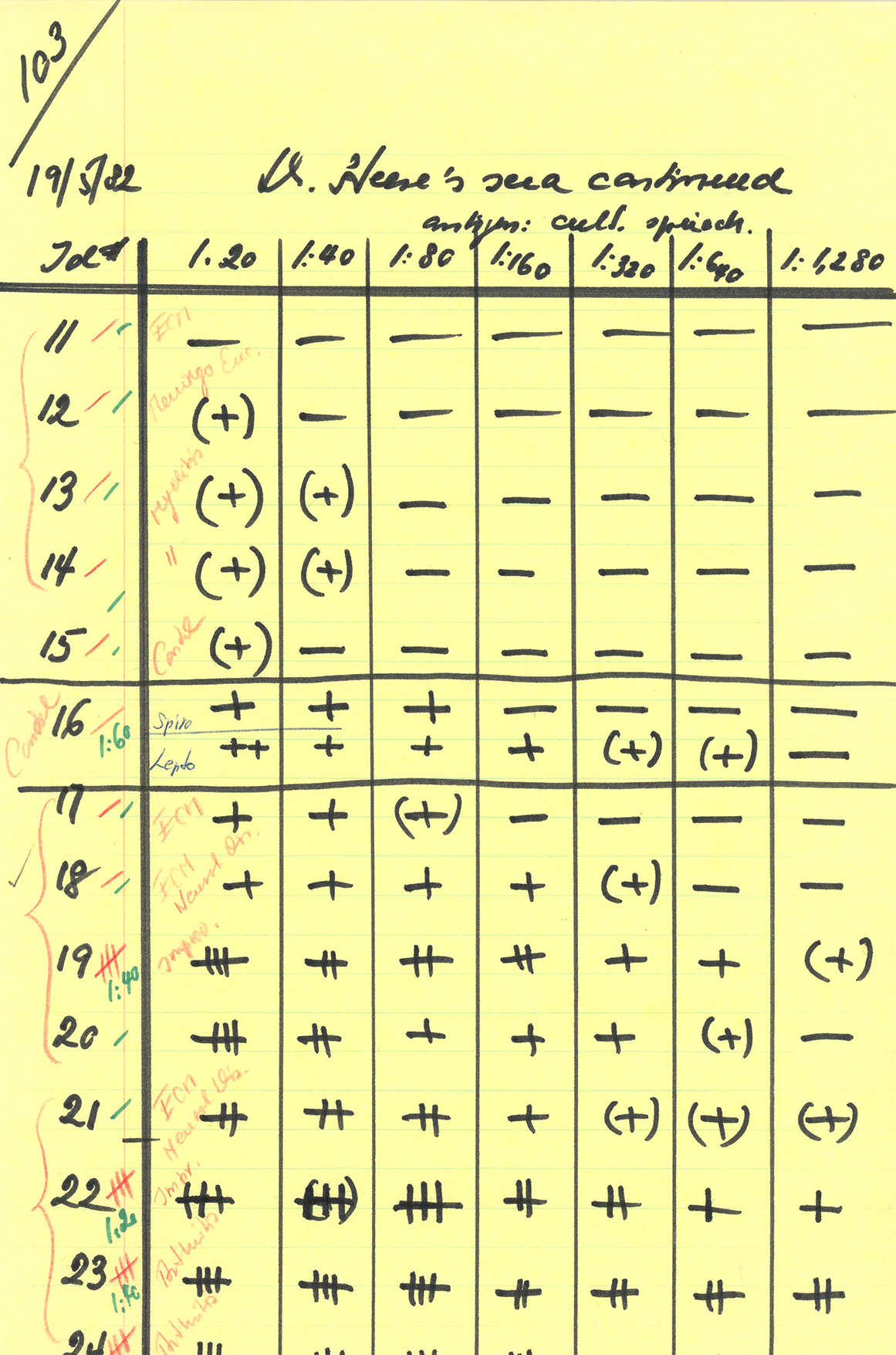
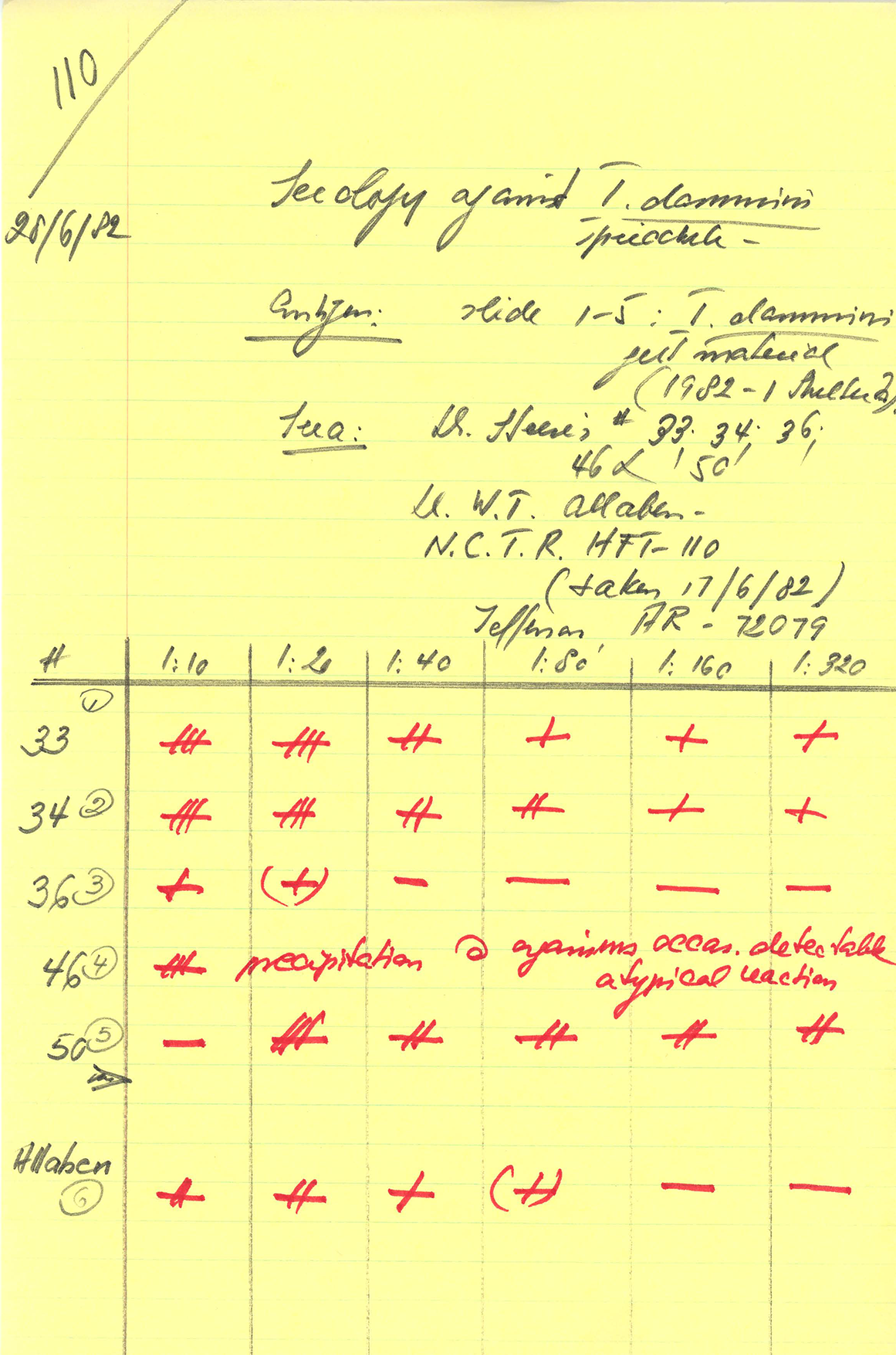
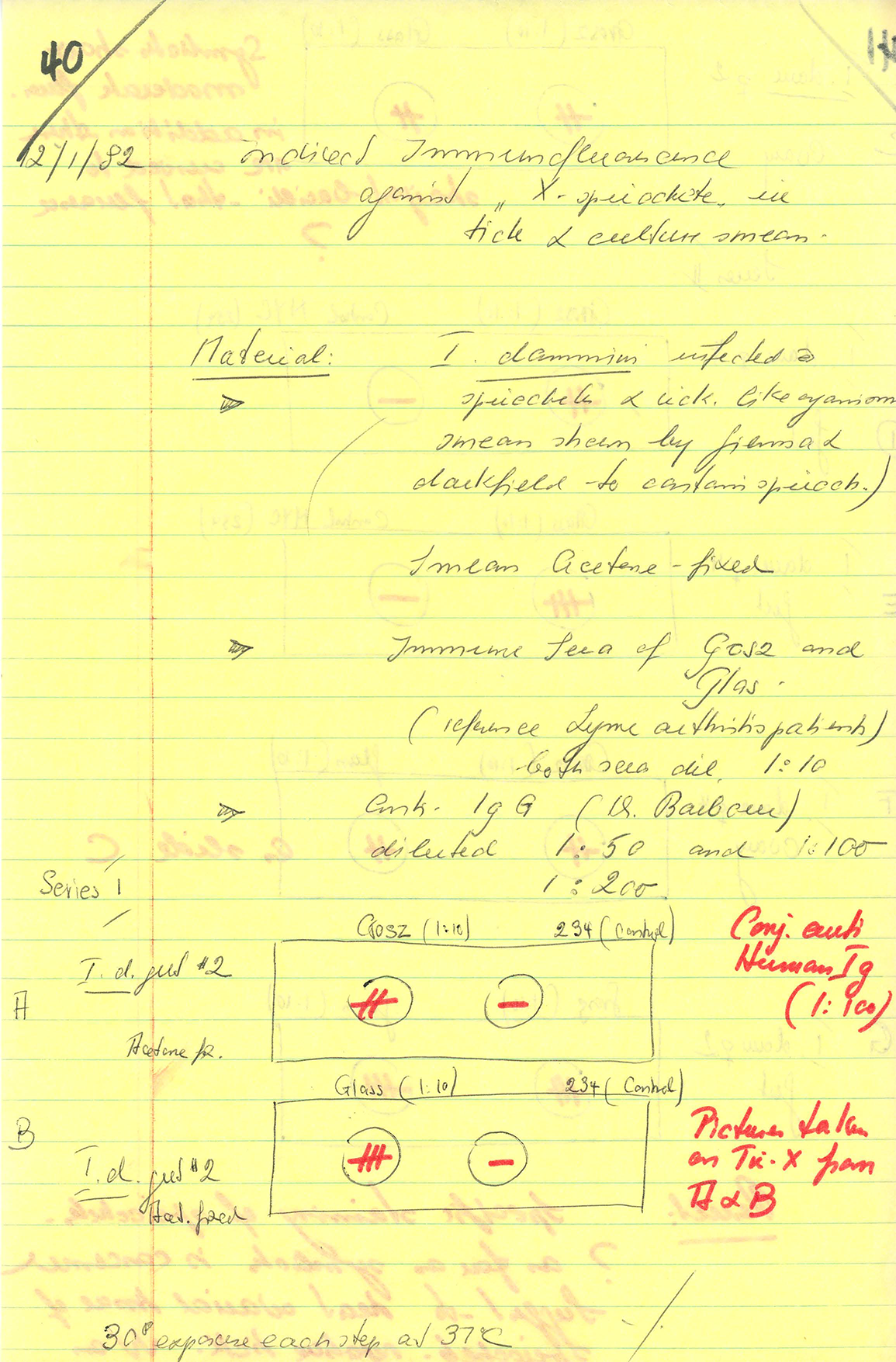
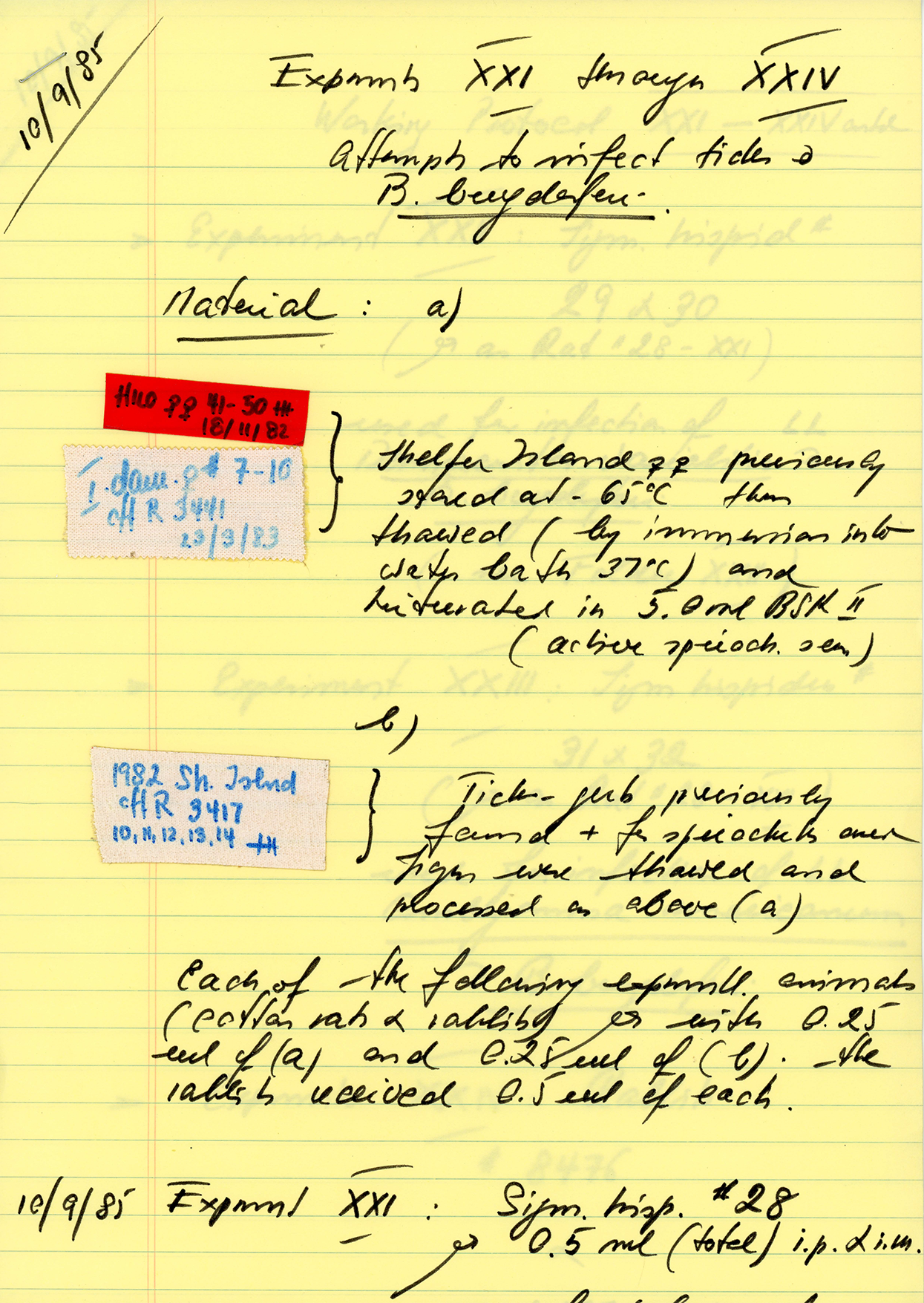
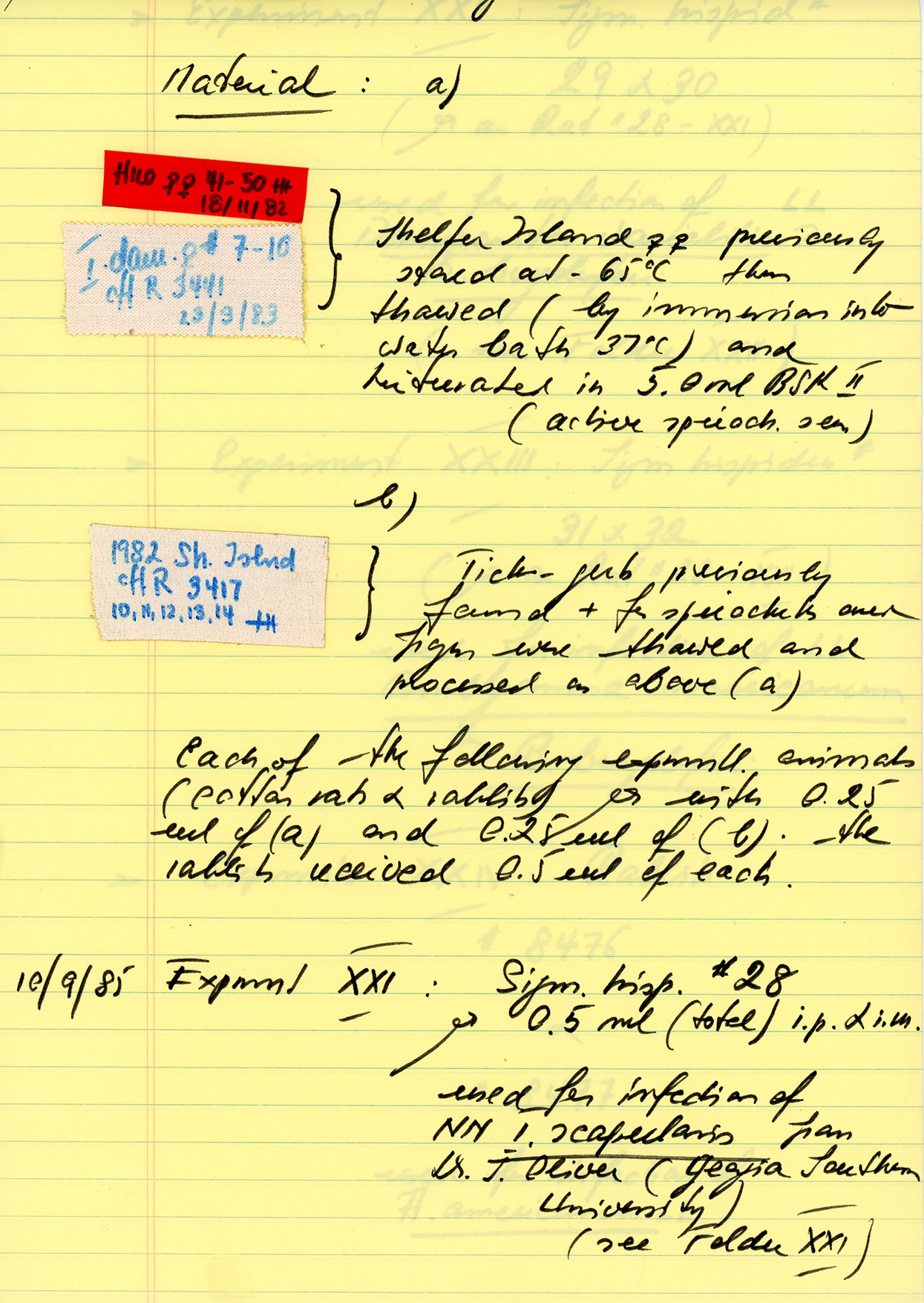
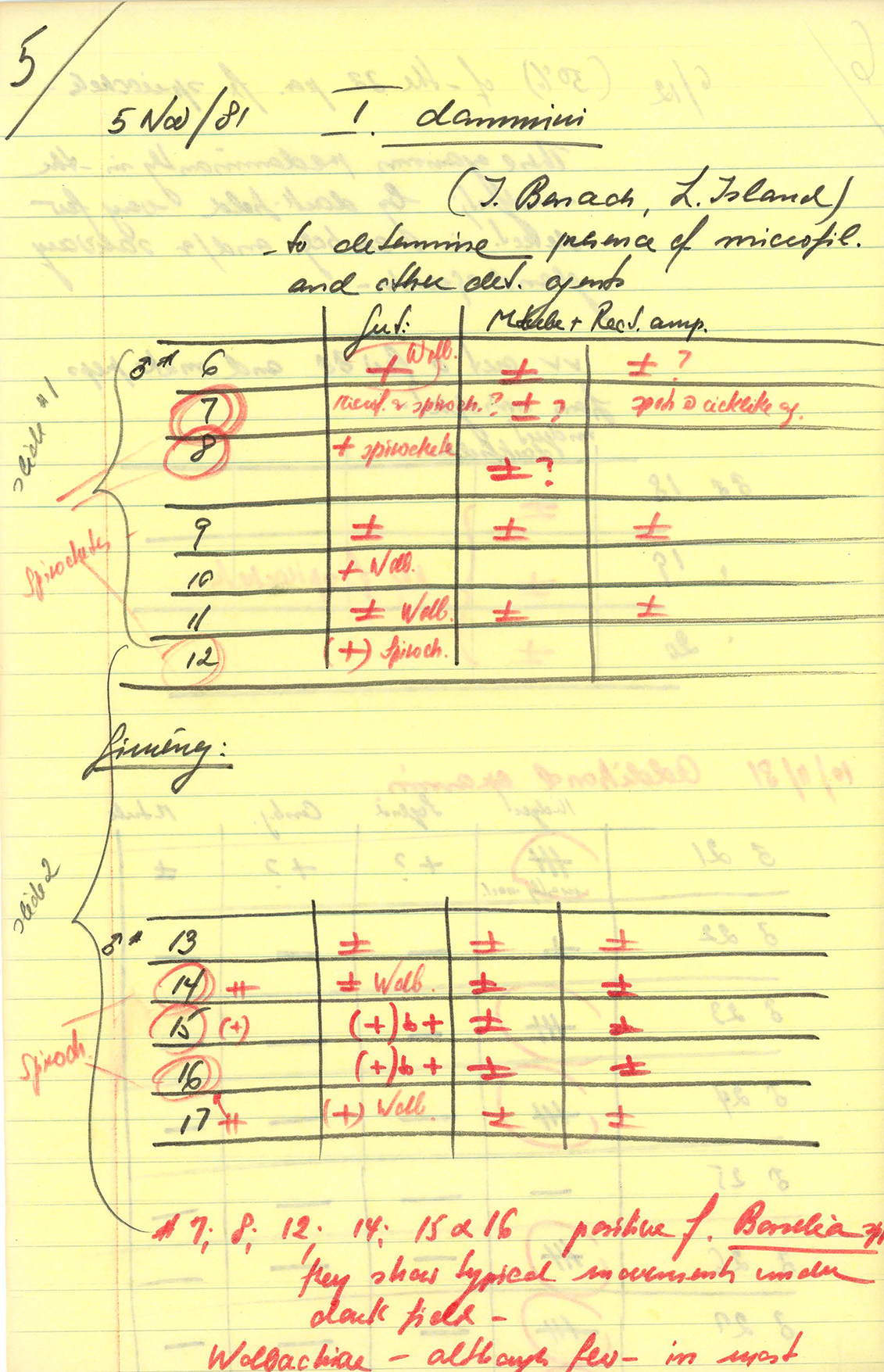
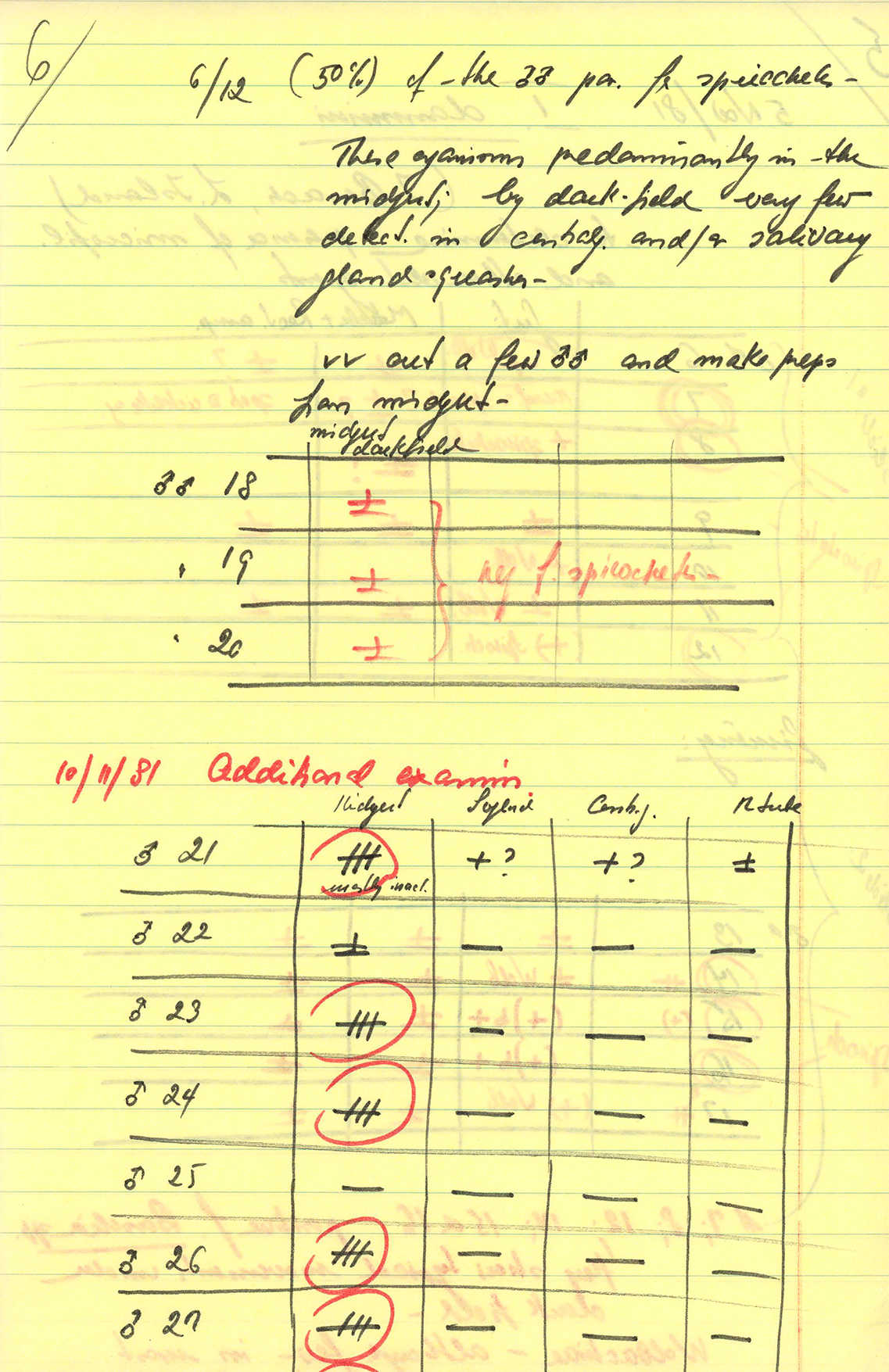
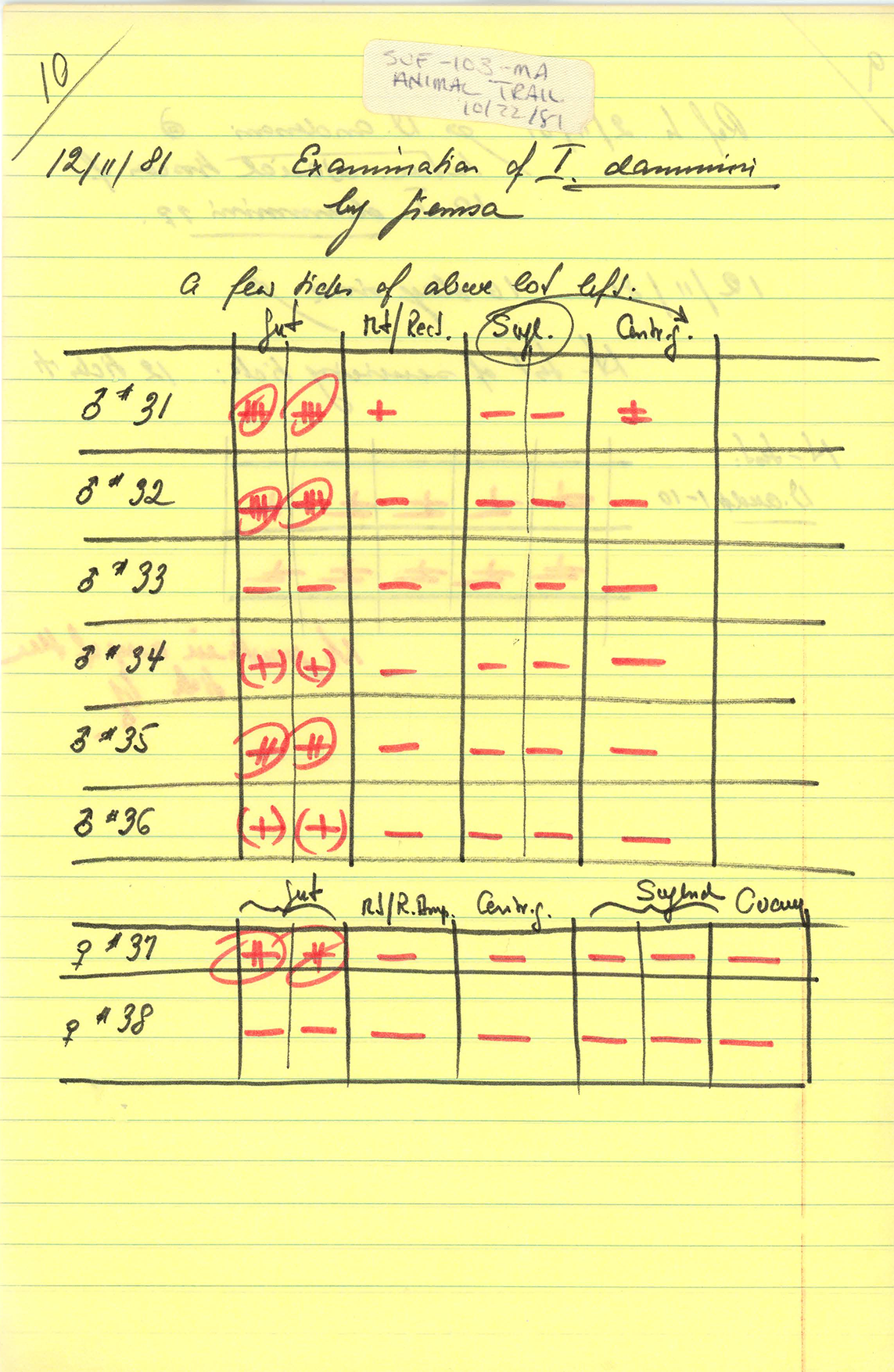
Charitably we could assume that Doug Wine omitted some words here, and intended to say “all blacklegged/deer ticks.” If that were the case, there is one spot in the country where Lyme infection rates among adult deer ticks approached those numbers: on Shelter Island — the place where the bacterium was first identified — approximately 66 percent carry Lyme. We also have to assume Dr. Wine is rounding up, to make this statement accurate.
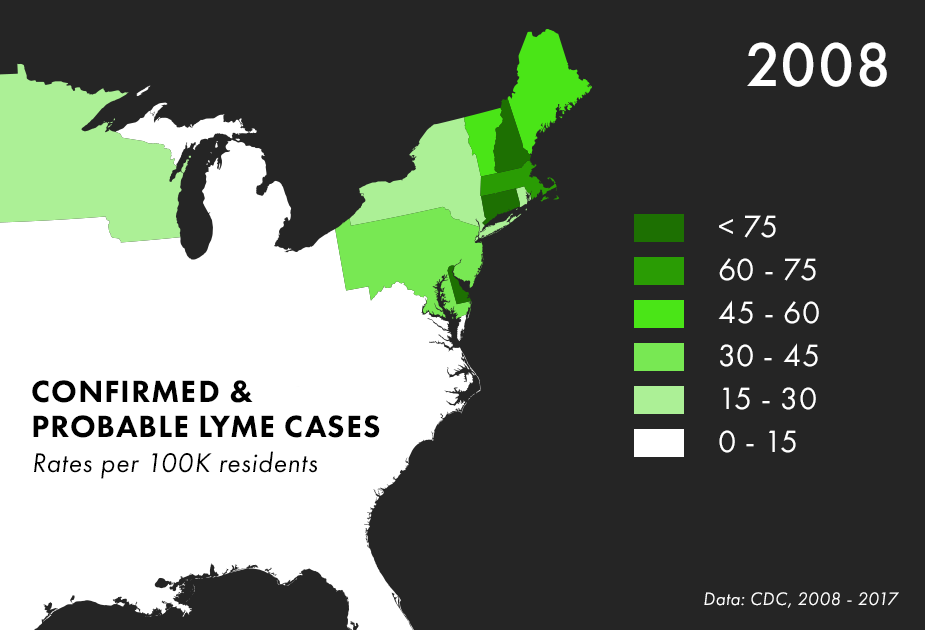
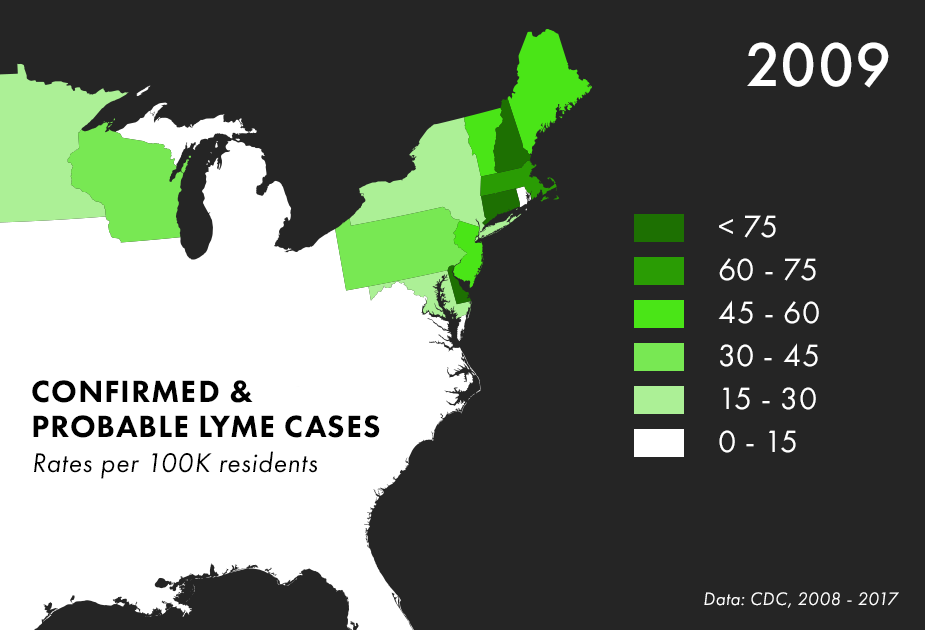
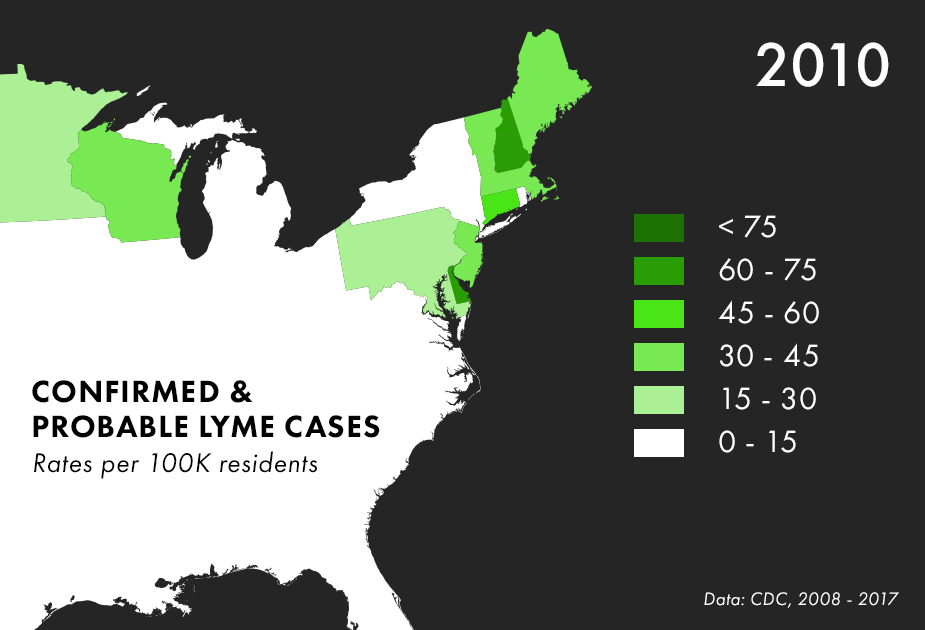
Across the whole country, infection rates among blacklegged ticks are closer to 20 percent. Even in the Northeast, where the epidemic is most acute, only around 25 percent of ticks carry the disease. In a recent nationwide study, Connecticut took the top spot at 30 percent.
These numbers are only referring to infection rates in blacklegged ticks, as we start to include dog ticks, western blacklegged ticks, lone-star ticks, and the other ninety tick species found in North America, Doug Wine’s statement becomes even less accurate.
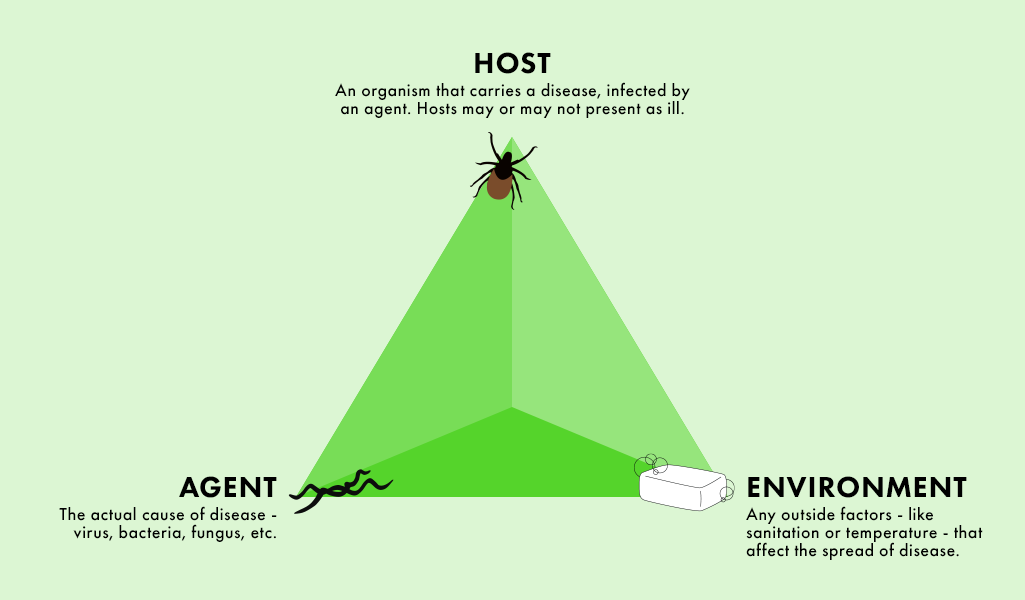
Statement: “The tick is, like, number 7 or 8 down the list of what is actually transmitting disease.”
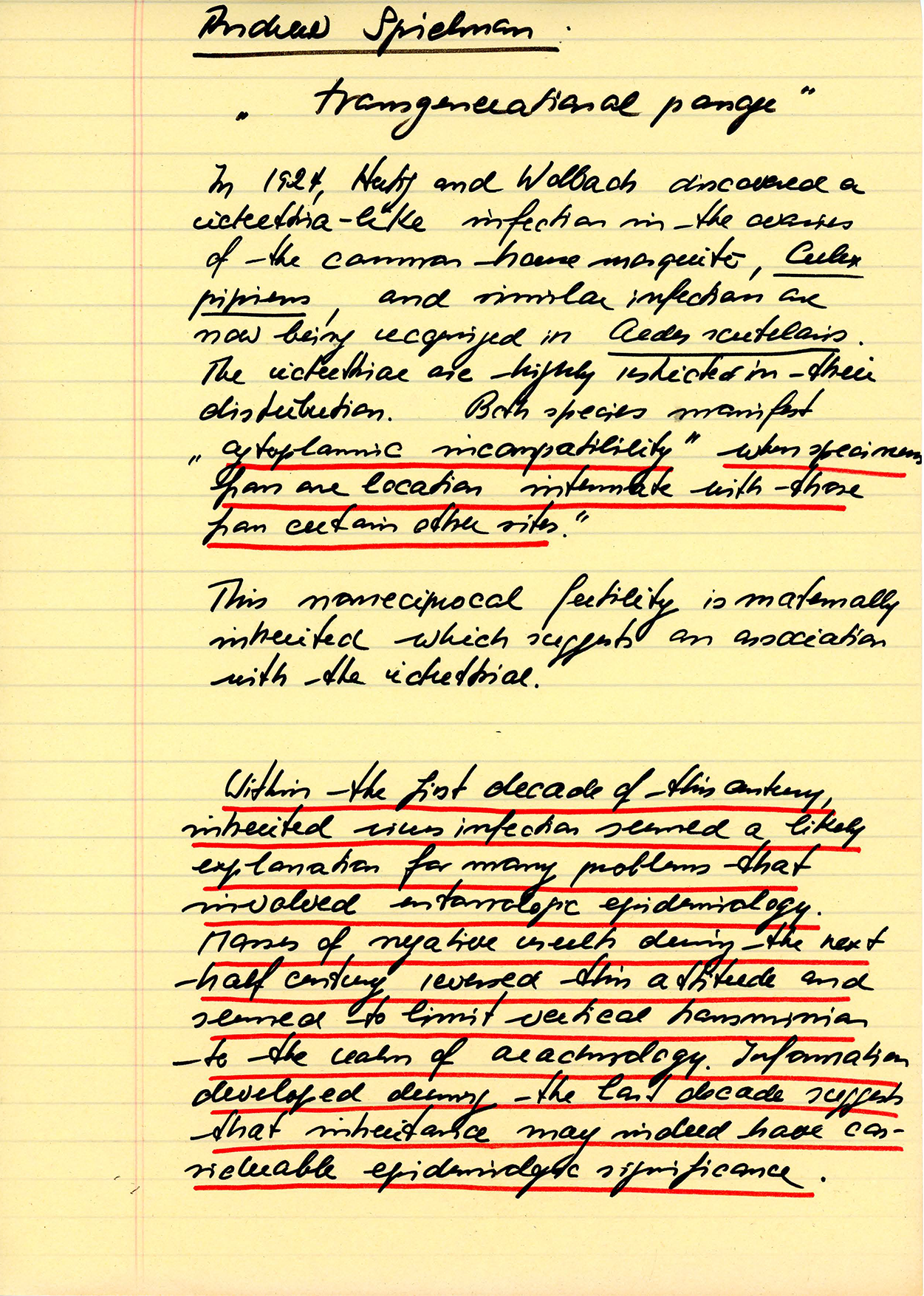
One study has found Lyme in mosquitoes, deer flies and horse flies. However, the same researchers attempted to transmit the disease from the mosquitoes to hamsters in a lab, and it didn’t work. Dog ticks can also be found to be carrying the Lyme pathogen, but have never been documented as transmitting it.
Enough googling will yield a single “case study” from Finland in which a man believes he contracted Lyme after being bitten by a deer fly, however this single case could also be explained by a tick bite that the jogger never noticed.
Statement: “Now we know that [Lyme disease] is sexually transmitted. We know that it is transmitted by all bodily fluids. You kiss someone, you have sex with someone you're giving it or getting Lyme disease.”
We’ll start with sex, and get to saliva next.
The root of this particular fallacy is a 2014 study that found Lyme disease in vaginal and seminal fluids. Further, syphilis is a spirochete, and is transmitted sexually, so why not Lyme?
The short answer is that detection of a bacteria in a fluid is not the same as proving it has evolved to transmit via that fluid. Syphilis creates open sores or chancres in and around the mouth and sexual organs, which produce large numbers of bacteria in order to facilitate transmission.
A 1991 study on infected rats designed specifically to test this question found no transmission of Lyme occurred through sex. A 1995 study of infected hamsters found the same. To date, there has been no recorded case of Lyme passing from person to person via sex or saliva - though there have been a few documented cases of Lyme being transmitted from mother to child through the placenta.
Statement: “Drink out of one bottle and you forgot which one is yours and you pick up the other one and have a drink of beer, and that guy has Lyme... You just acquired Lyme. One drop of saliva will do it.”
This statement — again — seems to flow from the 2014 study, though we could find no research confirming the presence of borrelia burgdorferi in saliva, only comments from fearful patients at the bottom of blog posts. However, even if it were present — again — this is not enough to ensure transmission.
HIV can be present in saliva as well, but that does not mean that you can get it through kissing.